When I got diagnosed with an ectopic pregnancy, I didn’t know much about this condition, what it actually meant, or what the treatment was like. Maybe you’re reading this because you’ve experienced or are experiencing ectopic pregnancy and in that case — I feel you. It’s my hope that this article can provide some help coping and support with your emotional and physical healing. Maybe you know someone who is in or has been through ectopic pregnancy, and you want to know more about what they are going through or how to support them. Or maybe you are just curious about this condition that we don’t seem to talk much about and for that I want to thank you. I appreciate your curiosity. Let us all be more curious and seek out knowledge! No matter what, my warm welcome to you. This article will take you through my own experience with ectopic pregnancy; the basics about what ectopic pregnancy is; the risk factors, symptoms, treatment procedures and the mental and physical recovery it often involves.
Before we begin, I want to remind you that a big part of this article is based on my personal experience and doctors’ evaluation of my specific case. As with pregnancy on the whole, all cases of ectopic pregnancy are different because our bodies, medical history and situations are all different. Always consult with a doctor yourself if you suspect or know you’re dealing with an ectopic pregnancy.
I’m pregnant?
When the doctor called me back into her office, I knew something was not quite right. “You’re pregnant,” she said. She sounded worried. “We need to get you to the hospital,” she added. I was 25 years old and had come in to have the doctor check my IUD. I had been bleeding a little for over a week, which wasn’t normal for me in the three years I’d had the IUD. Having the doctor tell me I was pregnant (or even to take a pregnancy test), was a bit of a shock to me. It hadn’t even occurred to me that I might be pregnant. Fortunately, I was not very far along and wasn’t experiencing any abnormal pain, so the hospital scheduled me for the following day. A positive pregnancy test while having an IUD can indicate ectopic pregnancy, which can be quite serious and potentially life-threatening. That’s why my doctor wanted to get me to the hospital right away. I never imagined that I would experience an ectopic pregnancy. I barely knew what it actually meant. But I do now.
What is ectopic pregnancy?
Ectopic pregnancy is when an ovum (a human egg) is fertilized and grows outside the uterus. “Ectopic” means “in an abnormal place or positionexternal link, opens in a new tab,” which is exactly what it is — the pregnancy is growing outside the uterus (abnormal) instead of inside the uterus, where a pregnancy should be happening, and needs to be if it’s to have any chance of resulting in a birth.
In a normal pregnancy, the fertilized egg travels down the fallopian tube (more on these later) to the uterus, where it implants in the uterine lining. You can read more about basic reproduction in Human Reproduction: A Seafarer’s Guide. If this is a lot of new or funny-sounding words, I totally get it! Stay with me!
In an ectopic pregnancy, things are a little different; the fertilized egg typically implants in one of the fallopian tubesexternal link, opens in a new tab instead of continuing into the uterus. As the pregnancy grows, it can rupture and cause internal bleeding and in severe cases be deadly. Ectopic pregnancy also cannot result in a birth: a fetus needs to be inside the uterus to develop. You’re probably starting to understand why my doctor sounded so worried.
An increased risk of a pregnancy being ectopic existed because I had an IUD. Other risk factors, besides having an IUD, include advanced maternal age (which usually means being over 35), smoking, a previous ectopic pregnancy, and assisted reproductive technologies use (Mummert & Gnugnoli, 2023external link, opens in a new tab). I was only 25 years old, not a smoker and had no prior history of ectopic pregnancy. It’s rare, but it happens. Ectopic pregnancy is less rare than you might think: it actually happens in around 1-2% of all pregnancies (NCBI2external link, opens in a new tab). Although this might sound low, that’s a lot of people worldwide! And this just makes it so much more important to talk about. If discovered early, severe consequences such as infertility or maternal death can be prevented and you can go on to live a normal life. Just like me. We need more easily accessible information about ectopic pregnancy. So here we are!
As we now know, ectopic pregnancy is when a fertilized egg implants outside the uterus, most often in the fallopian tubes (I promise, I’ll get to these soon!), which is not considered safe. Because ectopic pregnancies cannot be carried to term and can endanger the pregnant person if they continue to develop, they also demand treatmentexternal link, opens in a new tab. When diagnosed with an ectopic pregnancy, treatment is required, and depending on your situation — sooner rather than later. In some cases the body might naturally abort (by way of a kind of miscarriage where the body absorbs the tissue) the fertilized egg, however you would still need to be monitored closely by doctors. In most cases, an ectopic pregnancy will require treatment with medication or surgery. It isn’t possible to move the fertilized egg from the fallopian tube to inside of the uterus.
Like I said, finding out I was pregnant, even though I had an IUD, was not something I was expecting. However, the positive pregnancy test didn’t necessarily mean that the pregnancy was ectopic. I spent the following few days after my doctor’s appointment going back and forth for more tests at the hospital, including ultrasounds and blood tests. In the first ultrasound examination, the doctors had trouble finding the pregnancy, and told me it was possible that my body naturally aborted the fertilized egg. To monitor or test for a pregnancy, the hCG level is measured. HCG stands for human chorionic gonadotropin and can be described as a pregnancy hormone — the higher the levels of it in a body are, the further along, or more developed, the pregnancy those hormones are there because of is. My hCG level kept increasing, indicating that the pregnancy was growing. After a couple of days it was clear to the doctors that the pregnancy was implanted in my left fallopian tube: more than 90% of ectopic pregnancies occur in the fallopian tubes. I was officially diagnosed with an ectopic pregnancy. As this can be quite dangerous, the doctors gave me 5 hours to decide between medical treatment or surgery. This was another shock for me. And a big decision.
Symptoms
Besides light bleeding for about 10 days prior to my doctor’s appointment, I had no other unusual or noticeable symptoms. Common symptoms of ectopic pregnancy include:
- pelvic pain/discomfort or abdominal pain/discomfort
- nausea/vomiting
- lightheadedness
- and/or vaginal bleeding (Mummert & Gnugnoli, 2023)
Maybe you are thinking these could be symptoms of so many things, a regular period or a normal pregnancy! I know I have experienced all these symptoms in relation to my regular period. If you’re experiencing some or all of these symptoms, it doesn’t necessarily mean that you’re pregnant or that you are experiencing ectopic pregnancy. I think the most important thing is to be aware of any symptoms that are not normal for you. This is not always easy or obvious, especially if you’re going through other things at the same time. Notice what’s going on with your body and consult with a doctor if something is out of the ordinary for you.
Medical treatment or surgery?
In my case, I had the choice between medical treatment or surgery. This is not always the case. Depending on where the fertilized egg implanted, how far along the pregnancy is, if it has ruptured, your medical history and more, your healthcare providers will present you with your options, make their recommendations or have to schedule an emergency surgery.
When treated medically, an ectopic pregnancy is usually treated with a medicine called methotrexate. Methotrexate is injected into a muscle, in this case typically the gluteal muscles (glutes). The medicine interrupts the development of the fertilized egg, which is then absorbed by the body (AAFPexternal link, opens in a new tab). Methotrexate can only be used if the ectopic pregnancy hasn’t ruptured and the hCG level is relatively low. With higher levels of hCG, methotrexate can be given in two doses. Whether the medical treatment consists of a single dose methotrexate or two doses, the patient needs to be monitored closely and regular follow-up blood tests are a necessary part of the medical treatment. The injections are given at the hospital, whereafter you can go home and will come in for the regular check-ups. This process typically takes around 8 weeks, but can vary from person to person and from case to case. If the hCG level doesn’t decrease, this could indicate that the medical treatment is not working and surgical treatment can be necessary.
Together with your healthcare provider, you will figure out if you’re suitable for medical treatment. In some cases, for example patients with liver disease, alcoholism, or patients who are breastfeeding, medical treatment isn’t recommended. This is why you’ll have to talk to your healthcare provider about which treatment is appropriate for you. Medical treatment can be a great option for many. Research also shows that treatment with methotrexate doesn’t affect future fertility (NCBIexternal link, opens in a new tab). Common side effects of methotrexate are abdominal pain, vomiting, nausea, and vaginal bleeding. It is highly recommended to avoid drinking alcohol during the treatment and to wait at least three months before getting pregnant (or trying to) again. There might be other important information regarding medical treatment and recovery in each individual case, why it’s important to talk to your healthcare provider about it.
I did not want surgery. I don’t think anyone ever wants surgery. But in my case, the medical treatment seemed less accessible. I wasn’t able to attend the required follow-up checks in the following months, I was feeling unsafe with the medication (for personal reasons), and might have had increased chances of another ectopic pregnancy in the same fallopian tube, if not removed. So, I decided to have the surgery and be done with it. I do want to add that medical treatment is a great and safe option in many cases of ectopic pregnancy: it just wasn’t great for me.
A surgery to terminate an ectopic pregnancy and/or remove a fallopian tube is typically done with laparoscopy, where small incisions (0.5 inch) are made in the abdominal (lower stomach area) and operated with a tiny camera. This is less intrusive and therefore is often easier to recover from than a standard surgery. My surgery took less than an hour. Pretty smart and fast, if you ask me! Patients are under full anesthesia, like an induced deep sleep. It can feel scary, unfamiliar, new, worrying: I know, I was so nervous. So nervous, in fact, that the hospital staff let my sister go with me all the way into the operating room (OR).
The surgical team took out my left fallopian tube. I spent one night at the hospital and one week recovering in bed. Rest, healthy food, and community were some of the important factors in my recovery. It was important for me to talk about the ectopic pregnancy and my experience with my loved ones to process everything that had happened. It all happened so fast. To this day, I’m very grateful for all the loving words, thoughts, listening ears and wishes they provided me with. If you can find even one person who you can talk to and who can be there for you in the time around the treatment, this can really help! Having someone around you can do wonders for your healing. This might mean that you have to reach out to loved ones and be vocal about your situation. I’m not saying scream from the mountains (unless you want to), but it’s okay to ask for help and to talk about ectopic pregnancy.
Fallopian tubes are cool! Life after ectopic pregnancy
How is life with just one fallopian tube? This was a big question for me prior to my decision between medical treatment or surgery. Maybe you’re wondering the same thing.
I knew very little about fallopian tubes before this, so I started researching and asking the doctors. The more I learned, the more fascinated I became with these small but rather significant tubes connected to the uterus. What are they? The fallopian tubes, sometimes also called uterine tubes, are muscular tubes connected to each side of the uterus. They are around 4 inches long and less than 0.04 inches wide (NCBIexternal link, opens in a new tab). For those who born with them, there are typically two fallopian tubes.
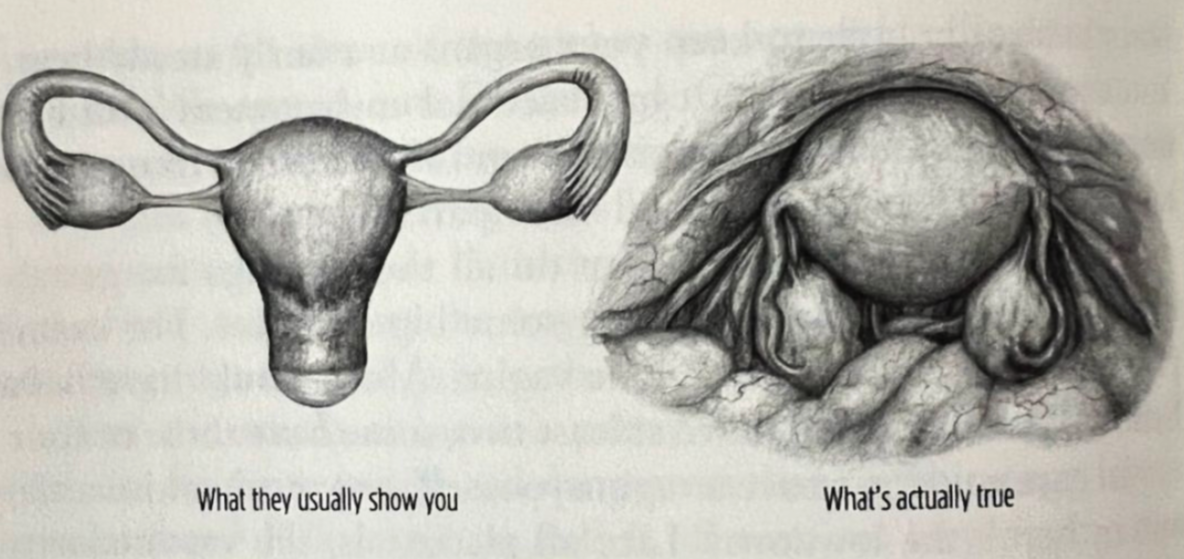
You might have seen the classic triangle shaped drawing of the pelvis of a person with a vulvovaginal reproductive system. If the triangle is the uterus, then the triangle’s arms are the fallopian tubes, and they hold on to two glands: the ovaries. In reality, this organ is much more compact, and folded closely together. The fallopian tubes run from the uterus to the ovaries (where the eggs are carried and matured). However, the fallopian tubes are not attached to the ovaries. The end of the fallopian tube, called the fimbriae (the part extended to the ovaries, that looks like small tentacles) can retrieve the egg from the ovary into its tube every month. This is ovulation.
When, for whatever reason, left with only one functional fallopian tube, the remaining tube can reach over and pull the mature egg from the opposite ovary. So, when one fallopian tube is removed, as in my case, the other tube can retrieve eggs from both ovaries. If this sounds like magic to you, I get it. It’s as close as it gets! Now, I want to mention that the ovaries don’t necessarily take turns ovulating every month. For example, ovulation can occur from the right ovary several months in a row and then switchexternal link, opens in a new tab. But because of this flexible fallopian tube, adjusting to my new normal, I now get my period every month and continually have the opportunity to get pregnant. Thank you, right fallopian tube!
Recovery and sex life
After the surgery, I was (understandably) exhausted and I spent one week with much bedrest, small walks, and little work. The following week, I had to come in for a follow-up to monitor that my body was recovering. They also gave me some medication to help my digestive system get back on track since I was feeling very constipated from the anesthesia (a common side effect of anesthesia, whatever it’s used for). It’s normal to bleed for one to two weeks after the procedure, because the body is disposing of the uterine lining, just like during menstruation.
During my first ultrasound scan, the doctoral team also took out my IUD (since it clearly wasn’t doing its job preventing pregnancy). Returning home after the surgery, I now had one less fallopian tube, and was no longer on any birth control, which I had been pretty consistently for 8 years. I was ready to learn about my natural menstrual cycle, and chose to learn about and follow the fertility awareness method (+ use of condoms). I took a break from sex, learning about my cycle and giving my body plenty of time to heal. It took me a while to get to know my (new) cycle and body, now that I was no longer on birth control (or pregnant). I somehow felt that my body betrayed me. Like we had a deal not to get pregnant and definitely not ectopically. My desire for sex was temporarily impacted by this experience, surgery and recovery. I wasn’t feeling very sexy for a while after, and my desire was lower than my normal. In time, I slowly started to explore sex with my partner again. It was important for me to talk about taking it slow, now that my body and I felt a little bit different than before. Slowly, I introduced different types of intimacy and sex into my life again.
I now have four small (tiny) scars from my belly bottom and down. They remind me about a scary and unpredictable experience and also all the love and care I received and gave to myself. Dealing with ectopic pregnancy is not easy and it presents some serious risks and consequences. However, the body is a pretty extraordinary system and can get through it with the right time and the right help. There might be other circumstances influencing your situation that I cannot speak to, or that are different than my experience was. Please always consult with your doctors and other professionals. This is just my own humble experience. If you seek more information, the following websites can provide a more extensive in-depth explanation of the anatomy and medical procedures.
More on ectopic pregnancy:
- Ectopic pregnancy FAQexternal link, opens in a new tab
- Ectopic pregnancyexternal link, opens in a new tab
- The anatomy of fallopian tubesexternal link, opens in a new tab
- Anatomy, Abdomen and Pelvis: Fallopian Tubeexternal link, opens in a new tab
